Scientists have long known that clumps of misfolded proteins, called aggregates, accumulate in the brains of people who suffer from neurodegenerative conditions such as Alzheimer’s and Parkinson’s diseases.
Aggregates of certain proteins, such as alpha-synuclein and beta-amyloid, are particularly associated with the development of Parkinson’s disease (PD). For example, alpha-synuclein aggregates create deposits in the brain called Lewy bodies, which eventually lead to the destruction of dopamine neurons that is associated with the condition.
Early diagnosis
Currently PD can only be diagnosed after physical symptoms start to develop, at which point many dopamine neurons have already been lost. Earlier diagnosis would mean more effective treatments could be given at an earlier stage of the disease.
Yu Zhang, who worked on this project for his PhD, says: “You want to be able to diagnose way before someone develops symptoms of the disease, when treatment can be more effective. We believe our new method might be able to do this.”
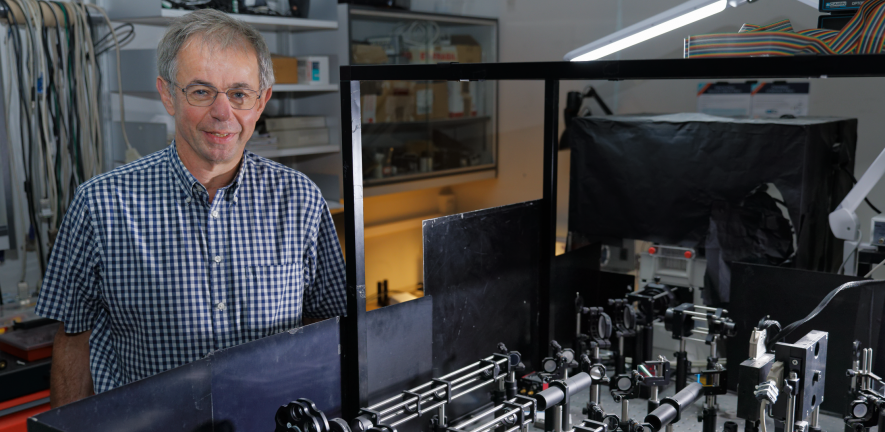
The problem until now has been the inability to easily and accurately measure the small amounts of aggregates in the blood and assess which characteristics will lead to Parkinson’s disease. To overcome this, Professor Sir David Klenerman and his team developed a new combined method which allows them to ‘fingerprint’ the aggregates in easily prepared blood serum samples.
A new technique
First the team used a highly sensitive and specific single-molecule imaging platform called single-molecule pull-down, through which they showed that the ratio of alpha-synuclein to beta-amyloid aggregates was higher in PD blood than control groups. They then used super resolution microscopy to measure the size and shape of the aggregates, and found that the aggregates in PD blood tended to be larger and rounder. They combined the two techniques to develop the biomarker.
David says: “Aggregates have been very challenging to study because they are at very low concentrations, and so selectively capturing them and measuring them in the blood is a real technical challenge. With our new tool we can measure size and shape and also identify different aggregates such as those of the Tau protein, which is also associated with Alzheimer’s disease. There is no complex processing, we can simply dilute the serum sample and stick it on the slide. It’s a technical tour de force.”
A new biomarker
The researchers applied the new technique to human blood serum from patients who had been diagnosed with PD for no more than one year, and compared the results with samples from non-PD patients. They found that the ratio of alpha-synuclein aggregates to beta-amyloid aggregates was higher in the PD serum than in the control group. Additionally, the PD serum had a higher portion of larger and rounder a-syn aggregates than the controls. By combining these two metrics together they achieved a very high diagnostic accuracy.
Next steps
The combined technique is called APSiMPull. The researchers have recently been awarded a three-year MRC grant for £1M to continue their work. They believe the technique could also be used to find biomarkers in Alzheimer’s and other neurodegenerative diseases.
“We are looking forward to continuing our strong collaboration with the clinicians Dr Caroline Williams-Grey and Professor James Rowe at the Cambridge Biomedical Campus,” says David. “They are the ones who see the patients and provide insight, and they have been very generous in giving us the samples we need. We are also very grateful to the patients who have provided blood and lumbar samples.”
This article first appeared in Chem@Cam magazine Winter 2023 Issue 67 pg 20.

