The researchers, led by Professor Sir David Klenerman of this department and Professor Caroline H. Williams-Gray from the Department of Clinical Neurosciences, used a technique developed in the Klenerman Lab called aptamer DNA-Paint, to count and image protein aggregates in the blood.
Using this technique, they were able to discriminate early Parkinson’s disease cases from a healthy control group with an accuracy of 98.2 percent.
A miniature "DNA paintbrush"
Proteins are the essential building blocks of life in human cells. Proteins can form larger clusters called aggregates, which occur naturally in our brains, cerebrospinal fluid (CSF) and blood. The body’s clearance systems normally keep these aggregates under control, maintaining a healthy ‘protein homeostasis.’
However, for unknown reasons, protein aggregates can build up in the brain, CSF and bloodstream and overwhelm the body’s coping mechanisms. Some aggregate build-up is part of the normal ageing process, but certain aggregates such as alpha-synuclein and amyloid beta are associated with neurodegenerative disorders such as Parkinson’s and Alzheimer’s disease.
In a paper published in Brain, the researchers describe how they used the new technique to measure aggregates of alpha-synuclein and amyloid beta in the blood and CSF of early-stage Parkinson’s disease patients and a control group.
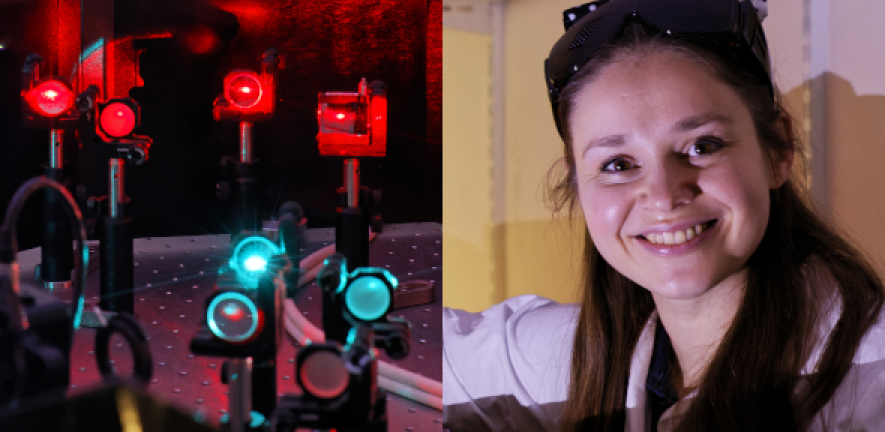
The method works like a miniature “DNA paintbrush” by repetitively “painting” the aggregates with fluorophore-labelled DNA. By determining the location of the DNA when bound to the aggregate, the researchers can build up a super-resolution image of the aggregates present in blood samples.
Astonishingly clear
The results were astonishingly clear. The researchers found that alpha-synuclein aggregates in blood were larger in Parkinson’s disease patients than in the healthy control group. They also found that the proportion of alpha-synuclein to amyloid beta aggregates in blood was significantly increased in patients with Parkinson’s disease, from 30 percent to 50 percent. Combined with other techniques and statistical analysis, the researchers were able to discriminate early Parkinson’s disease cases from the control group with an accuracy of 98.2%.
Previously, scientists lacked the tools to effectively count and measure protein aggregates in the blood, due to their extremely low concentration, which can be as little as one part per billion. The new aptamer DNA-paint technique allowed them to gradually build up an image of the size and shape of the alpha-synuclein and amyloid beta aggregates within the blood serum samples.
“Most people would not believe that this was a feasible experiment,” says Klenerman, who holds a Royal Society GSK Research Professor in this department and is also based at the UK Dementia Research Institute. “Blood is an incredibly complicated sample, so the fact we can see the aggregates in blood and image their size is quite amazing.”
“We’re basically pushing the boundaries. We measured the aggregates in CSF first, but surprisingly we did not see a clear difference between CSF in the Parkinson’s disease group and the control group. We then decided to try the same technique in blood. The idea was let’s see what’s possible and not possible, and—surprisingly--we found it is possible.”
Potential blood test
The ability to measure which aggregates in the bloodstream are a clear indicator of Parkinson’s disease is a real breakthrough, because it opens up the possibility of a diagnosis at a much earlier stage of the disease than ever before possible. Klenerman explains: “The early diagnosis would be very powerful; it means you could treat people before the disease develops. By the time people are treated now, they have usually already developed debilitating symptoms.”
The new technique may also lead to a better understanding of how and why aggregates form in the first place. “The key finding is that there are aggregates present in blood whose size and relative numbers we can now measure with excellent sensitivity and selectivity, and which correlate with Parkinson’s disease,” says Klenerman. “This research not only opens up early diagnostic potential, but now we can also start to understand how aggregates are formed in real humans rather than model systems.”
First author Dr Evgeniia Lobanova, a postdoctoral researcher in the Klenerman Lab, says next steps will include working on a simplified version of the test that can then be tried on a larger cohort. “We are also investigating other parameters that can be extracted from the data, such as those characterising the morphological features of aggregates to establish whether there is a difference in the shape of aggregates in people with Parkinson’s disease. We would also like to look at other protein aggregates implicated in the disease,” she says.
The new technique also has potential for the diagnosis of other neurodegenerative disorders such as Alzheimer’s disease.
Research

